Fat in Arteries Can Worsen Cardiovascular Problems
About Cardiac Arrest
Cardiac arrest occurs when the heart unexpectedly stops beating, usually because of abnormal heart rhythms, called arrhythmias.
Surprisingly, cardiac arrest most often strikes people in the prime of their lives–in their mid-30s to mid-40s. Victims may appear healthy before cardiac arrest and have no obvious symptoms of heart disease. But they typically have undiagnosed coronary artery disease (CAD) – the most common cause of the dangerous heart rhythm problems that can lead to this condition.
Other heart diseases that increase the risk for cardiac arrest include:
- heart failure (caused by the heart’s decreased pumping ability)
- inherited conditions that affect the heart
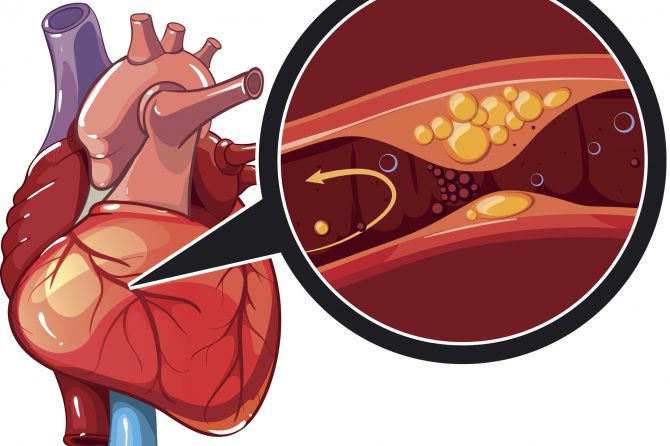
CAD occurs when fatty plaque deposits accumulate on the walls of the coronary arteries, which supply blood to the heart. Over time, the plaque buildup causes the coronary arteries to narrow. The plaque may rupture and form blood clots, which can cause heart attacks by limiting blood flow in the coronary arteries or by blocking them completely.
Scar tissue may replace the heart cells that die during a heart attack. The scar tissue can disrupt the heart’s electrical system and increase the risk of developing harmful arrhythmias.
Physicians may prescribe beta-blockers or other medications to help lower the risk for cardiac arrest in people who have severe CAD or who have suffered a recent heart attack. Some people may also need angioplasty or coronary artery bypass surgery to improve blood flow to the heart.
Implantable cardioverter defibrillator devices, which detect and respond to dangerous heart rhythms, are another option doctors may consider in certain high-risk patients, including those who have already experienced cardiac arrest.
People with CAD or other heart conditions should see their physicians regularly and follow their treatment plans. Healthy habits may also help reduce the risk for cardiac arrest:
- Choose a balanced diet of nutritious foods that are low in saturated fat, trans fat, cholesterol, salt, and added sugar.
- Shed excess weight.
- Exercise as regularly as possible, preferably at least 30 minutes a day on five or more days each week.
- Quit smoking.
Always consult your physician or other healthcare provider for more information.
Some people with abnormal fatty deposits in their arteries are at higher risk than others for heart attack, stroke, and cardiovascular death, a new study shows.
The fatty condition, referred to as atherothrombosis, puts people at increased risk for heart attack and stroke stemming from reduced blood flow from the artery blockage.
The large, multi-center study is reported in the Journal of the American Medical Association (JAMA) and was presented at a recent meeting of the European Society of Cardiology in Sweden.
SECTION HEADER
Dr. Deepak L. Bhatt, of Harvard Medical School, and his team studied 45,000 patients who were enrolled in the Reduction of Atherothrombosis for Continued Health (REACH) study.
Detailed information was gathered at the start, with additional annual follow-up at one, two, three, and four years.
The researchers found that patients with abnormal fatty deposits in an artery were at highest risk if they had a prior history of heart attack or other emergencies linked to an artery blockage.
They also discovered that of the participants studied, 81 percent had hypertension, 70 percent had high cholesterol levels in the blood, and nearly 16 percent had narrowing of the arteries in numerous locations.
In fact, 48 percent of the patients had prior heart attacks, unstable angina, or other problems related to the artery blockage. About 28 percent of those patients had such an event within the previous year.
Studies Provide Clues to Help Physicians
During the follow-up period, 5,481 patients experienced cardiovascular events that included 2,315 with cardiovascular death.
The researchers also found that 1,228 people with myocardial infarction (heart attack), 1,898 with stroke, and 40 with both a myocardial infarction and stroke occurring on the same day.
Among patients with atherothrombosis, those with a prior history of ischemic events at the beginning had the highest rate of new ischemic events, while patients with stable coronary, cerebrovascular, or peripheral artery disease had a lower risk.
Patients without known atherothrombosis, but with risk factors only, had the lowest risk of new ischemic events.
The researchers say this information can help physicians identify patients with various stages of atherothrombosis who are at high risk of future heart and vascular problems.
Always consult your physician or other healthcare provider for more information.
Online Resources
(Our Organization is not responsible for the content of Internet sites.)

Leave a reply